Medical microrobots that can travel inside your body are (still) on their way
Microrobots released into the body could bust up clots, deliver cancer drugs, and even guide listless sperm to their target.
This article first appeared in The Checkup, MIT Technology Review's weekly biotech newsletter. To receive it in your inbox every Thursday, and read articles like this first, sign up here.
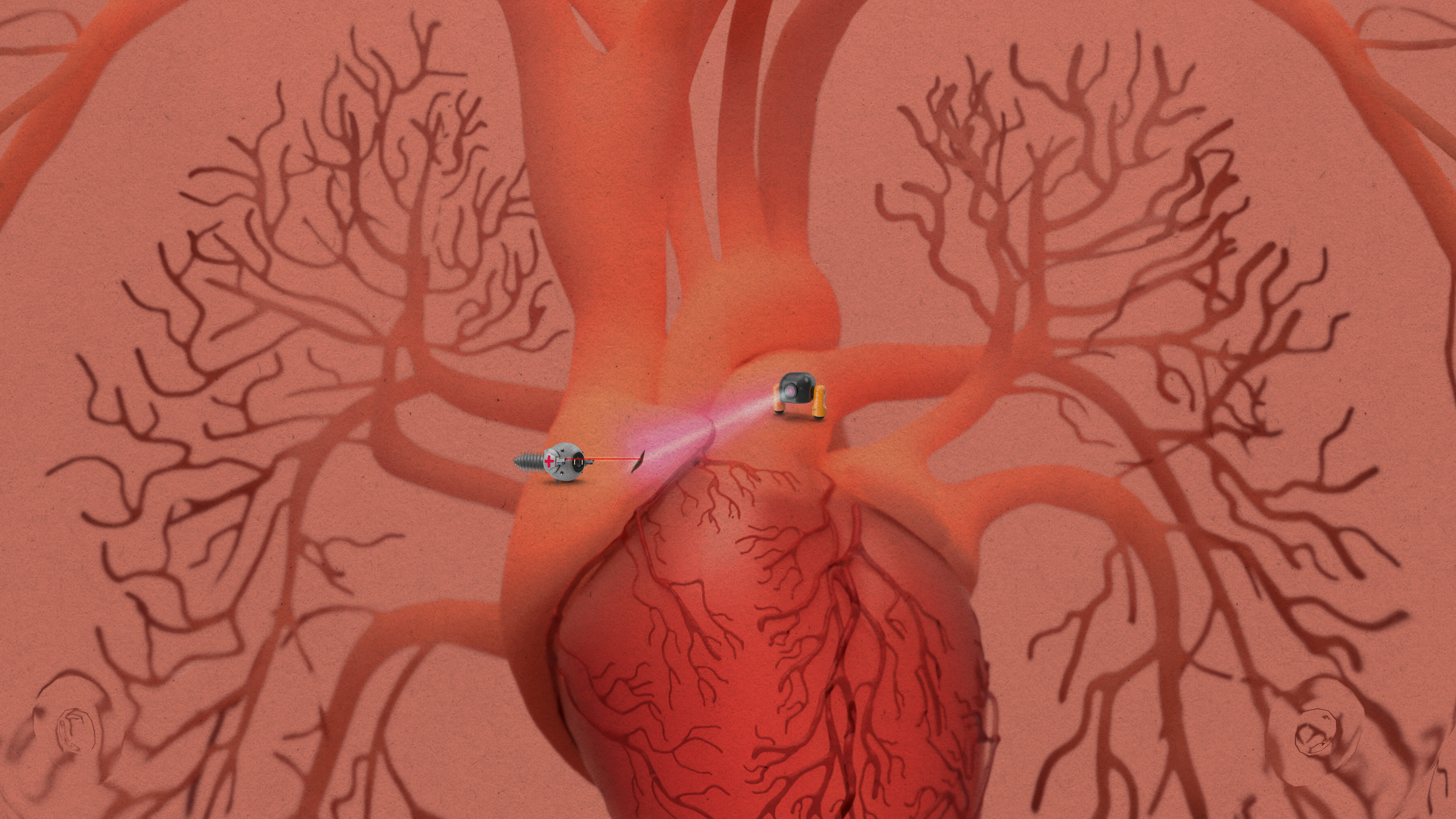
The human body is a labyrinth of vessels and tubing, full of barriers that are difficult to break through. That poses a serious hurdle for doctors. Illness is often caused by problems that are hard to visualize and difficult to access. But imagine if we could deploy armies of tiny robots into the body to do the job for us. They could break up hard-to-reach clots, deliver drugs to even the most inaccessible tumors, and even help guide embryos toward implantation.
Okay, I know what you’re probably thinking. We’ve been hearing about the use of tiny robots in medicine for years, maybe even decades. And they’re still not here. Where are my medical microbots already?
They’re coming, says Brad Nelson, who works in robotics at ETH Zürich. Soon. And they could be a game changer for a number of serious diseases. In a perspective published in Science today, Nelson and his coauthor Salvador Pané argue that these tiny machines could help deliver drugs exactly where they are needed. That would help minimize toxicity. “So we can use stronger doses and maybe we can rethink the way we treat some of these diseases,” Nelson says.
What makes Nelson optimistic that these technologies are on their way? Some such robots have made their way off the lab bench and into large animals, including pigs. There are at least four startups working on medical microrobots that could travel “untethered” inside the body. One of these, Bionaut, raised $43 million earlier this year to take its therapy into phase 1 trials. It will use the money to develop devices about the size of a pencil tip that are designed to deliver drugs to the site of glioma brain tumors and pierce cysts that block the flow of spinal fluid in the brain, a symptom of a rare childhood disorder called Dandy-Walker syndrome.
“Microrobot” is a catch-all term covering robots that range in size from one micron (about 100th of the width of a human hair) up to a few millimeters in scale. If the robot is really tiny, smaller than a micron, it’s a nanorobot. And while it may be enticing to say “microbot” because it sounds really cool, that’s “more of a Hollywood kind of term,” Nelson says.
Microrobots can be composed of synthetic materials, biological materials (these are called biological robots or biobots), or both (biohybrid robots). Many of them, including the ones that Nelson is developing, move thanks to magnets.
But others can move on their own. Last week a team of researchers from Tufts and Harvard reported that they had turned tracheal cells into biobots. The human trachea has waving cilia on the inside to catch microbes and debris. But these researchers encouraged the tracheal cells to form an organoid with the cilia on the outside. Depending on their shape and cilia coverage, the bots could travel in straight lines, turn circles, or wiggle. And—surprise twist—when the researchers scraped a metal rod across a layer of living neurons growing in a dish, the biobots swarmed the area and triggered new neurons to grow. “It is fascinating and completely unexpected that normal patient tracheal cells, without modifying their DNA, can move on their own and encourage neuron growth across a region of damage,” said Michael Levin, an engineer at Tufts who led the work, in a press release. “We’re now looking at how the healing mechanism works, and asking what else these constructs can do.”
The potential usefulness of these microrobots is vast. “A lot of people are thinking about vascular diseases,” Nelson says. Microrobots could be injected and dissolve blood clots in the brain to treat stroke patients. Or they could shore up weak spots in vessels in the brain to prevent them from bursting. They could deliver drugs to specific locations. And then there are weirder applications. Researchers at the University of Pennsylvania have developed bots that they hope might one day replace your toothbrush.
Other teams are working on bots that mimic—or are made from—sperm. Researchers have developed cow sperm covered in iron nanoparticles, called IRONSperm, that swim with the help of a rotating magnetic field; the hope is that they can be used for targeted drug delivery. One team from Germany is working on microrobots that help with fertilization by delivering weakly swimming sperm to the egg. Their system even releases drugs to break down the egg’s hard coating. That same group also recently described how microrobots might be used in IVF. In a typical IVF procedure, an egg is fertilized outside the body, and the resulting embryo is transferred to the uterus. The procedure often fails. But if microbots could shuttle the embryo back to the fallopian tube or endometrium, the embryo could develop under more natural conditions, which might improve implantation rates. They envision microrobots guided by magnetic fields that could grip or carry an embryo, release it, and then degrade naturally.
Still, there are some substantial hurdles that the companies will have to overcome to use these bots in humans. Some are technical. “These are very tiny systems,” says Victoria Webster-Wood, a mechanical engineer at Carnegie Mellon University who develops biohybrid robots. And because of that, a bodily fluid like blood is actually relatively viscous. “So if the flow is moving really fast, it’s hard for the robot to go the other direction,” she says.
Other hurdles are regulatory. Microrobots qualify as medical devices, but they may also be delivering a drug. “You’ve got what’s called the drug-device combination,” Nelson says. “While the drug might be well known, its concentration is going to be hopefully significantly different than normal.” That might mean regulators will want to see additional studies.
Webster-Wood has been in the field for years, and she is excited that microrobots are finally getting attention. “Even in the last 10 years, it’s just grown so much,” she says. “I think there’s a lot more potential for actually translating.”
Another thing
This week the FDA is expected to approve Casgevy, the world’s first commercial gene-editing treatment, which treats sickle-cell disease. (The treatment was approved in the UK last month.) Antonio Regalado dug deep into the science behind the treatment for this story, which explains why sickle-cell was an ideal target for CRISPR’s big therapeutic debut.
Read more from Tech Review’s archive
We’ve been thinking about microrobots and medical robots for years. Way back in 2011, Kristina Grifantini covered what was then one of the central puzzles: how to control them.
Earlier this year, Antonio Regalado reported on the first babies conceived with robots and the startups working to automate IVF. These weren’t microrobots, and the goal was mainly to achieve scale. “The main goal of automating IVF, say entrepreneurs, is simple: it’s to make a lot more babies.”
Victoria Webster-Wood, who makes biohybrid robots, and Renee Zhao, who makes millimeter-scale medical robots both made this year’s Tech Review 35 Innovators Under 35 list.
From around the web
Brain implants helped five people with moderate to severe brain injuries perform 15% to 52% better on cognitive tests. If the results hold up in a larger study, brain stimulation may become the first therapy for traumatic brain injury. (NYT)
Last week the FDA announced that the agency was investigating a possible link between CAR-T therapy and cancer. If CAR-T can cause secondary cancers, it would be a rare occurrence, experts say. (STAT $)
Vets are on a quest to pinpoint the cause of a mysterious respiratory illness that has sickened hundreds of dogs in the US. (Wired $)
The surge in respiratory illness among kids in China is likely the result of a lengthy lockdown, not a new pathogen, as some Republican lawmakers have claimed. (NYT)
Deep Dive
Biotechnology and health
The Biggest Questions: What is death?
New neuroscience is challenging our understanding of the dying process—bringing opportunities for the living.
I received the new gene-editing drug for sickle-cell disease. It changed my life.
As a patient enrolled in a clinical trial for Vertex’s new treatment, I was among the first to experience CRISPR’s transformative effects.
The lucky break behind the first CRISPR treatment
Gene editing for sickle-cell is here. This is how researchers knew what DNA to change.
The first gene-editing treatment: 10 Breakthrough Technologies 2024
Sickle-cell disease is the first illness to be beaten by CRISPR, but the new treatment comes with an expected price tag of $2 to $3 million.
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.