Three people were gene-edited in an effort to cure their HIV. The result is unknown.
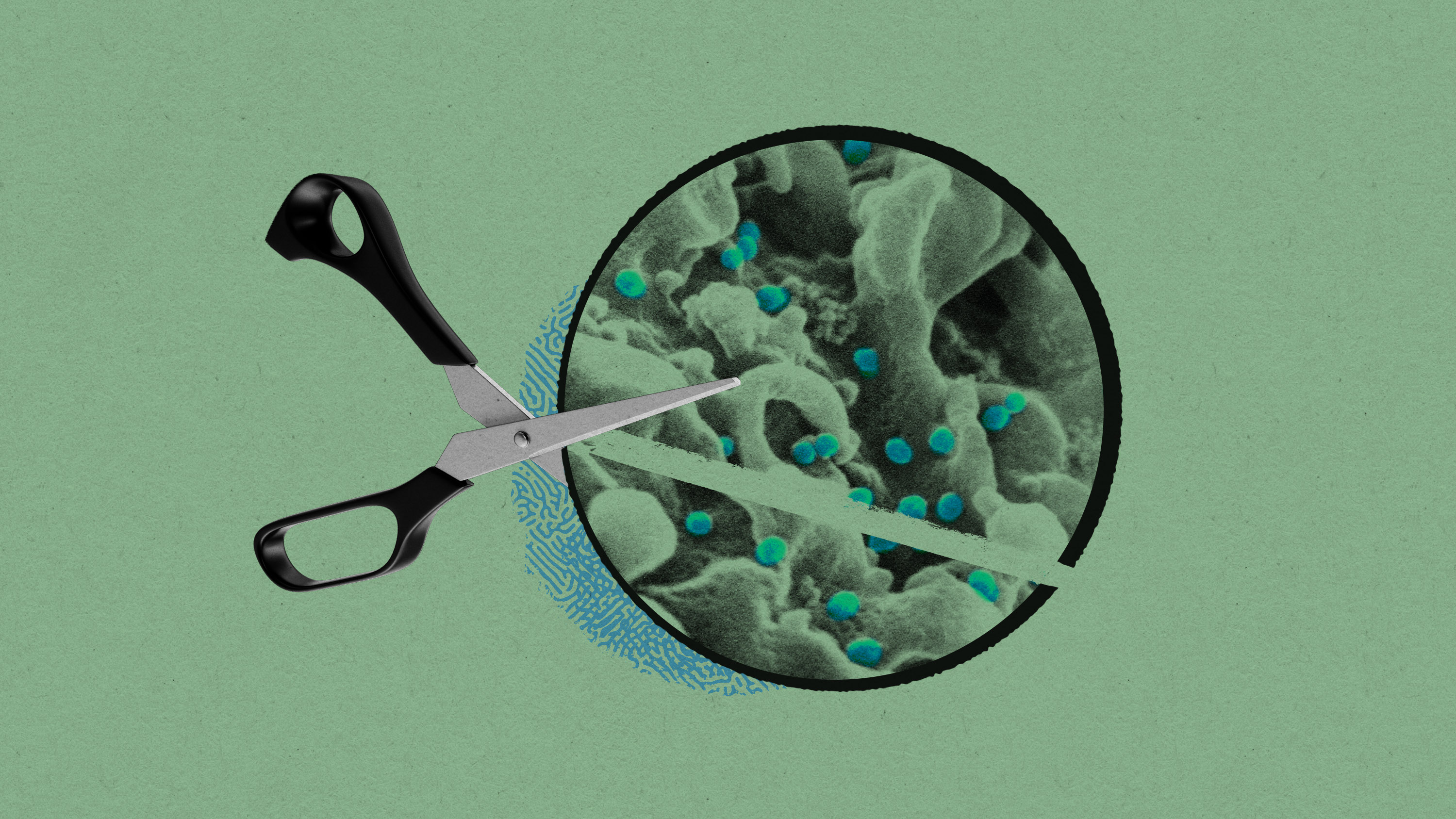
CRISPR is being used in an experimental effort to eliminate the virus that causes AIDS.
The gene-editing technology CRISPR has been used to change the genes of human babies, to modify animals, and to treat people with sickle-cell disease.
Now scientists are attempting a new trick: using CRISPR to permanently cure people of HIV.
In a remarkable experiment, a biotechnology company called Excision BioTherapeutics says it added the gene-editing tool to the bodies of three people living with HIV and commanded it to cut, and destroy, the virus wherever it is hiding.
The early-stage study is a probing step toward the company’s eventual goal of curing HIV infection with a single intravenous dose of a gene-editing drug. Excision, which is based in San Francisco, says the first patient received treatment about a year ago.
Today, doctors involved in the study reported at a meeting in Brussels that the treatment appeared safe and did not have major side-effects. However, they withheld early data about the treatment’s effects, leaving outside experts guessing whether it had worked.
“This is an exceptionally ambitious and important trial,” says Fyodor Urnov, a genome-editing expert at the University of California, Berkeley, who believes it “would be good to know sooner than later” what the effect was—“including, potentially, no effect.”
A failure wouldn’t come as a surprise to anyone familiar with HIV. It has proved a devious adversary: there is still no vaccine, even 40 years after the virus was identified in 1983.
Still, pharmaceutical companies did develop antiretroviral drugs, which stop the virus from copying itself. Taking these pills lets people with HIV live normal lives. But if they stop, the virus will quickly rebound and, if left unchecked, cause the fatal syndrome of infections and cancers known as AIDS.
Hidden virus
One reason the virus can’t be fully wiped out with drugs alone is that it inserts its genetic material into the DNA of our cells, leaving behind hidden copies that can restart the infection.
“All of a sudden, the cell finds—Oh my god there’s a segment incorporated, and it’s the whole viral gene,” says Kamel Khalili, a professor at Temple University, who helped start Excision.
Vaccine makers have also struggled because HIV kills the very immune cells meant to stop infection. But a decade ago, Khalili says, he realized that CRISPR might offer a way to cure the infection without involving the immune system: by deleting the virus’s genes from their hiding places.
“If the viral gene is in your DNA, it becomes like a genetic disease,” he says. “And so you could use a genetic tool.”
Borrowed from nature
CRISPR technology was first developed in 2012 and was based on the discovery of molecules that bacteria use to spot and destroy incoming viruses, known as phages. It was quickly adapted to cut human DNA, launching the current era of human genome editing.
Most gene-editing studies getting attention today are those looking to treat inherited diseases, caused when people are born with faulty DNA. Exposing people to CRISPR can correct or remove those genes; one such treatment, for sickle-cell disease, is expected to win approval later this year.
Excision’s study is unusual in that it instead attempts to use gene editing to eliminate viruses. Among more than 50 gene-editing studies in human volunteers tallied by MIT Technology Review this year, only two involved infectious disease.
However, Khalili notes that zapping viruses was CRISPR’s original purpose in the wild. “Although the concept of using CRISPR against a virus looks novel, it stems from what was going on in nature already,” he says.
Initial lab tests showed that CRISPR could find and destroy the HIV genes in cells and, later, that it was able to functionally cure close to 40% of HIV-infected mice treated with a gene-editing drug dripped into their veins, says Khalili.
The company won permission to begin human tests, and so far, three people have received the treatment. Each got an IV drip that released billions of harmless viruses carrying DNA instructions for making, and aiming, the CRISPR scissors.
According to Excision, the treatment hasn’t caused major side effects. Given that it appears safe, the company said that it would continue the study with higher doses of the treatment next year, with six more patients getting three and then 10 times the amount delivered so far.
Does it work?
What is still missing is data on whether the treatment worked. Patients in the study were taking antiretroviral drugs, but the plan was for doctors to stop those drugs 12 weeks after the gene-editing treatment and see whether the virus rebounded or not—a step known as “analytical treatment interruption.” If the virus didn’t return, it could mean CRISPR had destroyed the viral genes.
For two of the patients, treated months ago, it appears the data is already known to the company. But William Kennedy, senior vice president of clinical development at Excision, said the third patient was treated only recently and that the full results for this group would not be reported until 2024.
That’s a long time to wait, given how fast gene editing is moving. But Urnov says gene-editing companies have become especially cagey because of a difficult financial environment. Some companies have seen their stock prices slide, and one, Beam Therapeutics, laid off 20% of its staff last week and said it would reorganize its efforts.
Khalili, who is not involved in Excision’s clinical trial and doesn’t have firsthand knowledge of the results, says the study could be just one step in a longer journey to a cure—one that could eventually involve combining multiple strategies.
“Even if we don’t completely cure [HIV], we might be getting a significant delay in the rebound of the virus,” he says. “That could set us up for the next stage, like any drug where there are first and second generations.”
Correction 11/2/2023: The percentage of mice that achieved a functional cure from HIV after receiving a gene-editing treatment in laboratory experiments was close to 40%. The original version of this article incorrectly gave the figure as 20%.
Deep Dive
Biotechnology and health
The Biggest Questions: What is death?
New neuroscience is challenging our understanding of the dying process—bringing opportunities for the living.
I received the new gene-editing drug for sickle-cell disease. It changed my life.
As a patient enrolled in a clinical trial for Vertex’s new treatment, I was among the first to experience CRISPR’s transformative effects.
The lucky break behind the first CRISPR treatment
Gene editing for sickle-cell is here. This is how researchers knew what DNA to change.
Medical microrobots that can travel inside your body are (still) on their way
Microrobots released into the body could bust up clots, deliver cancer drugs, and even guide listless sperm to their target.
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.